WHAT IS GBS?
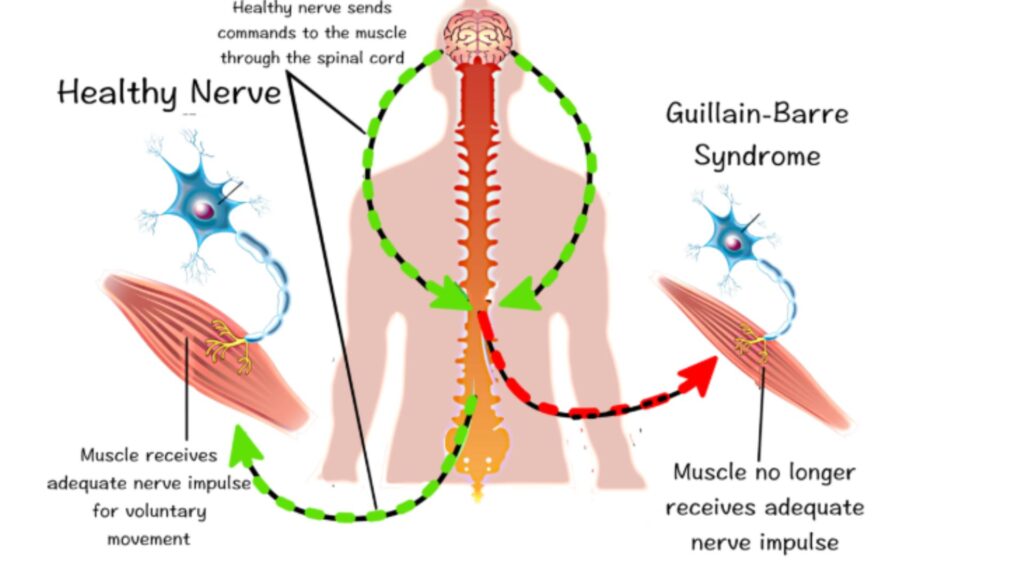
- Guillain-Barré syndrome (GBS) is a rare but serious post-infectious immune-mediated neuropathy. It results from the autoimmune destruction of nerves in the peripheral nervous system causing symptoms such as numbness, tingling and weakness that can progress to paralysis.
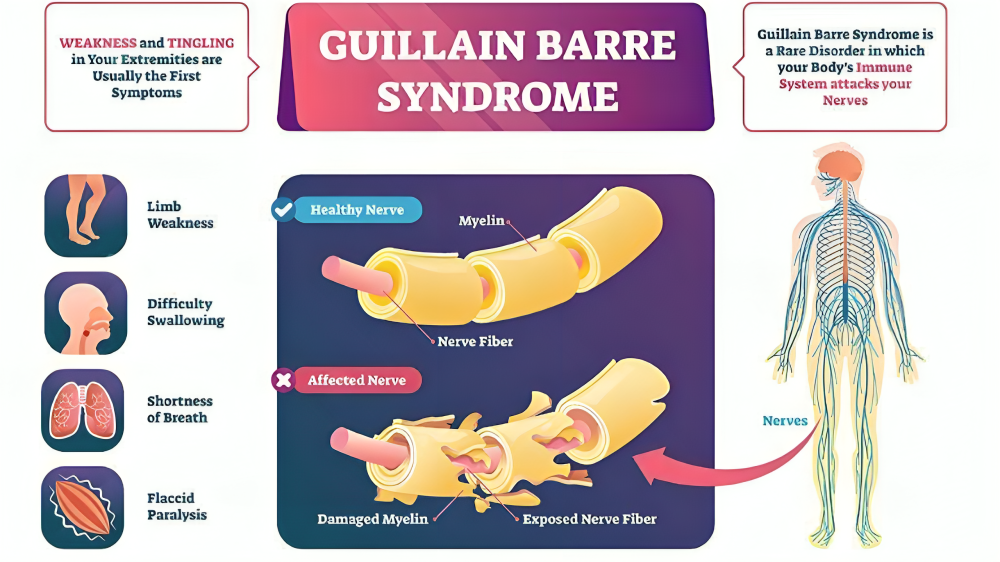
- Peripheral nerves contain long axonal extensions that transmit information these axons are protected by a layer of insulation called myelin. The type of peripheral nerve damage found in Guillain-Barré can be axonal, demyelinating, or both.
- The syndrome can affect the nerves that control muscle movement as well as those that transmit pain, temperature and touch sensations.
- While most patients recover with timely medical intervention, some may experience lingering symptoms.
- People of all ages can be affected, but it is more common in adults and in males.
- In AIDP and most other forms of Guillain-Barré Syndrome, both sides of the body tend to be equally affected.
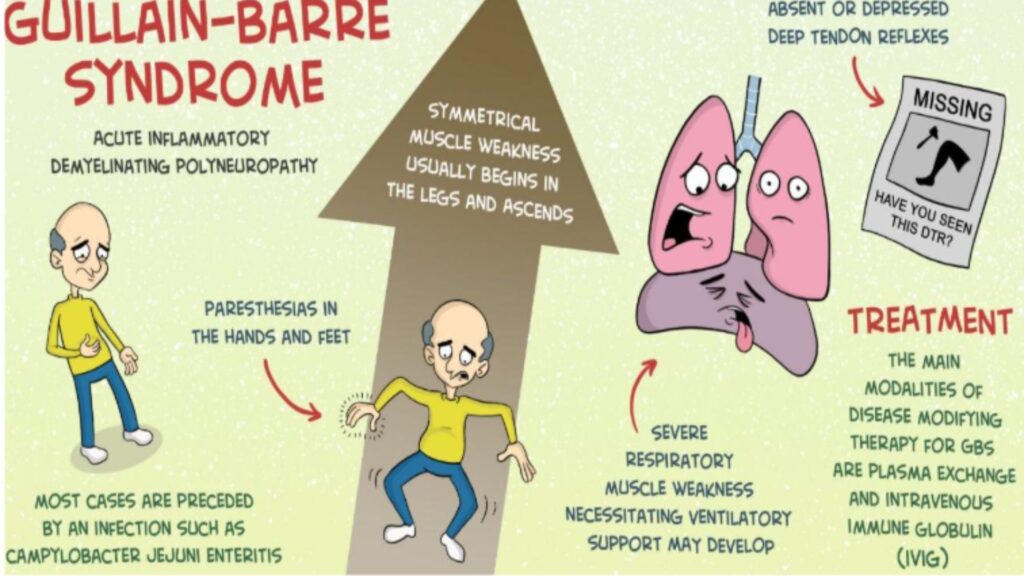
- Evidence from animal models suggests a key role of molecular mimicry. The most common organism which results in GBS is Campylobacter jejuni it contains a lipooligosaccharide present in the outer membrane of the bacteria is similar to gangliosides which are components of the peripheral nerves.
TYPES OF GBS:
1. Acute Inflammatory Demyelinating Polyneuropathy (AIDP):
Acute Inflammatory Demyelinating Polyneuropathy (AIDP) is the most common subtype of GBS although, overall, it’s a rare disorder that occurs in one out of every 1,00,000 people. In AIDP, antibodies don’t attack the nerve cells directly. Instead, they damage the glial cells that surround the axon of the nerve.
2. Acute Motor and Sensory Axonal Neuropathy (AMSAN):
In AMSAN, antibodies do not attack the myelin sheath or glial cells; instead, they damage the axon directly. They do this by attacking nodes, places along the nerve where the myelin breaks to allow ions to flow and pass along electrical signals. AMSAN can be very aggressive. Symptoms progress rapidly and can lead to total paralysis of all four limbs in fewer than seven days along with severe muscle wasting.
3. Acute Motor Axonal Neuropathy (AMAN):
AMAN accounts for fewer than 10% of GBS cases. Only nerves controlling movement are affected. This results in weakness of the lower arms and legs, but there is no numbness. People tend to recover more rapidly and completely from AMAN than the other forms of Guillain-Barré.
4. Miller-Fisher Variant:
Miller-Fisher is a rare variant of GBS that is associated with problems of the head and face rather than with limb paralysis.
Symptoms may include:
- Weakness or paralysis of the eye muscles
- Inability to swallow and/or speak
- Loss of tendon reflexes
- Respiratory complications
CAUSES:
- The exact cause of Guillain-Barré syndrome isn’t known. It usually appears days or weeks after a respiratory or digestive tract infection. Rarely, recent surgery or vaccination can trigger Guillain-Barré syndrome.
- Guillain-Barré syndrome may be triggered by:
- Most commonly, an infection with campylobacter, a type of bacteria often found in undercooked poultry
- Influenza virus.
- Cytomegalovirus.
- Zika virus.
- Hepatitis A, B, C and E.
- HIV.
- Surgery.
- Trauma.
- Rarely, influenza vaccinations or childhood vaccinations.
- COVID-19 virus.
RISK FACTORS:
- GBS can affect anyone of any sex or age, but most often affects adults and people older than 50.
- Infection with the bacteria Campylobacter jejuni, which causes gastroenteritis (including symptoms of nausea, vomiting and diarrhoea), is one of the most common risk factors for GBS.
SYMPTOMS:
- Muscle Weakness: Typically begins in the legs and ascends to the upper body.
- Numbness and Tingling: Often starts in the toes and fingers.
- Unsteady Walking: Difficulty walking due to muscle weakness.
- Difficulty with Eye or Facial Movements: Including speaking, chewing, or swallowing.
- Severe Pain: That may feel achy or cramp-like, most commonly in the back, legs, or arms.
- Bladder and Bowel Dysfunction: Such as difficulty in controlling urination or bowel movements.
- Rapid Heart Rate: Also known as tachycardia.

DIAGNOSIS:
Clinical Evaluation:
- Healthcare providers typically diagnose Guillain-Barré syndrome based on symptoms and medical history.
- Physicians also do physical and neurological exams to look for signs of muscle weakness and weak or absent deep-tendon reflexes (hyporeflexia or areflexia).
- However, many other neurological conditions share the same symptoms as GBS.
Diagnostic Tests:
- Lumbar puncture (spinal tap): A procedure to collect cerebrospinal fluid, which may show an elevated protein level without an increase in white blood cells.
- Electromyography (EMG): EMG Measures the electrical activity of muscles and can reveal nerve dysfunction.
- Nerve conduction velocity test (NCV): This test measures the nerve’s ability to send a signal. In GBS, the signals traveling along the damaged nerves are slowed because of damage to the myelin sheath. NCV assess the speed and strength of electrical signals traveling through the nerves.
TREATMENT:
Guillain-Barré Syndrome (GBS) treatment is mainly aimed at supporting the patient while treating the supernatural response of the immune system and preventing complications. The treatment of GBS include:
- Supportive Care, Pain Management, Nutritional Support, Physiotherapy
- Respiratory Support: In cases where the patient progresses to respiratory failure secondary to muscular weakness, they may require mechanical ventilation.
- Plasma Exchange (Plasmapheresis): This therapy involves filtering the blood to eliminate damaging antibodies that might be attacking the nerves. The blood cells are separated from the plasma, and the patient’s plasma is then replaced with a substitute. This lessens the severity and duration of the illness, mainly when done in the early stage of the disease.
- Immunoglobulin Therapy (IVIg): IVIg is the infusion of antibodies collected from thousands of healthy donors. This treatment has the potential to help modulate the immune system and reduce the assaults on peripheral nerves. It is less invasive than plasmapheresis, which is why it is mainly preferred.
Prompt diagnosis & intervention are critical for improving outcomes & reducing the severity.
Conclusion:
Guillain-Barré Syndrome is a rare but serious autoimmune condition that requires prompt medical attention. While most patients recover with appropriate treatment, early intervention is critical in preventing severe complications. Advances in immunotherapy and supportive care have improved outcomes significantly, but ongoing research is crucial to understanding the condition better. Raising awareness about GBS can help in early diagnosis, leading to better prognosis and quality of life for affected individuals.




